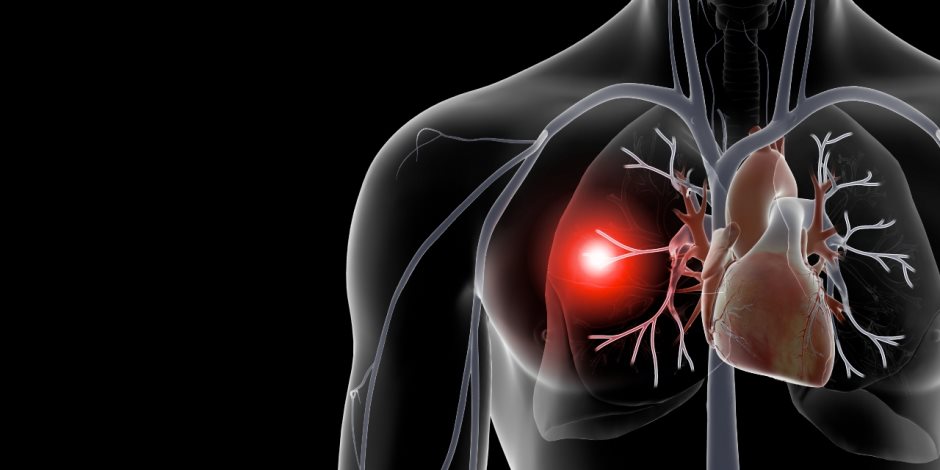
Pulmonary embolism is a blockage in one of the pulmonary arteries in the lungs. In most cases, pulmonary embolism is caused by blood clots that travel to the lungs from the legs or, rarely, other parts of the body (deep vein thrombosis).
Because the emboli block blood flow to the lungs, pulmonary embolism can be life-threatening. However, prompt treatment greatly reduces the risk of death. Taking measures to prevent blood clots in your legs will help protect you against pulmonary embolism.
SYMPTOMS
- Shortness of breath. This symptom typically appears suddenly and always gets worse with exertion.
- Chest pain. You may feel like you’re having a heart attack. The pain may become worse when you breathe deeply (pleurisy), cough, eat, or bend. The pain will get worse with exertion but won’t go away when you rest.
- Cough. The cough may produce bloody or blood-streaked sputum.
- Leg pain or swelling
- Discolored skin (cyanosis)
- Fever
- Excessive sweating
- Rapid or irregular heartbeat
- Lightheadedness or dizziness
When to see a doctor
Pulmonary embolism can be life-threatening. Seek immediate medical attention if you experience unexplained shortness of breath, chest pain or a cough that produces bloody sputum.
CAUSES
Pulmonary embolism occurs when a clump of material, most often a blood clot, gets wedged into an artery in your lungs. These blood clots most commonly come from the deep veins of your legs. This condition is known as deep vein thrombosis (DVT).In most cases, multiple clots are involved but not necessarily all at once. The portions of lung served by each blocked artery are robbed of blood and may die. This is known as pulmonary infarction. It makes it more difficult for the lungs to provide oxygen to the body.Occasionally, blockages in the blood vessels are caused by substances other than blood clots, such as:
- Marrow fat from a broken long bone
- Collagen or other tissue
- Part of a tumor
- Air bubbles
RISK FACTORS
- Previous history of blood clots
- Family history of blood clots
- Clotting disorders
- Heart failure
- Certain cancers (especially pancreatic, ovarian & lung)
- Women with a personal or family history of breast cancer who are taking tamoxifen or raloxifene
- Surgery
- Smoking
- Being overweight
- Estrogen based birth control pills
- Hormone replacement therapy
- Pregnancy
- Prolonged immobility such as: Being confined to bed for an extended period after surgery, a heart attack, leg fracture, trauma or any serious illness.
- Long trips. Sitting in a cramped position during lengthy plane or car trips
COMPLICATIONS
Pulmonary embolism can be life-threatening. About one-third of people with undiagnosed and untreated pulmonary embolism don’t survive. When the condition is diagnosed and treated promptly, however, that number drops dramatically.Pulmonary embolism can also lead to pulmonary hypertension, a condition in which the blood pressure in your lungs and in the right side of the heart is too high. When you have obstructions in the arteries inside your lungs, your heart must work harder to push blood through those vessels. This increases the blood pressure within these vessels and the right side of the heart, which can weaken your heart.In rare cases, small emboli occur frequently and develop over time, resulting in chronic pulmonary hypertension, also known as chronic thromboembolic pulmonary hypertension.
TREATMENT
Treatment is aimed at keeping the blood clot from getting bigger and preventing new clots from forming. Prompt treatment is essential to prevent serious complications or death.
- Blood thinners (anticoagulants). These drugs prevent new clots from forming while your body works to break up the clots e.g. heparin, warfarin.
- Clot dissolvers (thrombolytics). While clots usually dissolve on their own, there are medications given through the vein that can dissolve clots quickly. Because these clot-busting drugs can cause sudden and severe bleeding, they usually are reserved for life-threatening situations.
- Clot removal. If you have a very large, life-threatening clot in your lung, your doctor may suggest removing it via a thin, flexible tube (catheter) threaded through your blood vessels.
- Vein filter. A catheter can also be used to position a filter in the body’s main vein – called the inferior vena cava – that leads from your legs to the right side of your heart. This filter can help keep clots from being carried into your lungs. This procedure is typically reserved for people who can’t take anticoagulant drugs or when anticoagulant drugs don’t work well enough or fast enough. Some filters can be removed when they are no longer needed.
THANKS FOR READING
Don’t forget to subscribe to get the latest updates. If you have any questions or suggestions, leave a comment below or contact me here.



